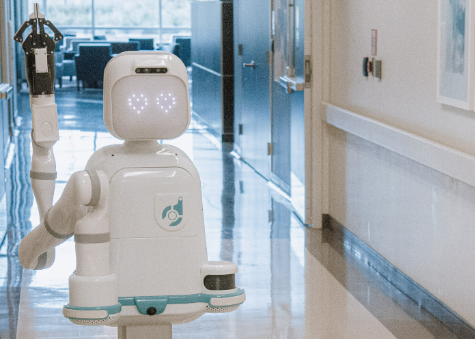
Robotic arms performing delicate surgery, AI diagnostics spotting tumors invisible to the human eye – the promise of medical robots feels like science fiction made real. Headlines tout increased precision, smaller incisions, and faster recoveries, painting a near-utopian future for healthcare. But is the story truly that simple? Beneath the gleaming surfaces and impressive demos lie significant, often overlooked Disadvantages of Medical Robots that impact patient care, hospital budgets, and the very fabric of medical practice. Before we fully embrace the robot revolution, it's crucial to understand these critical drawbacks that rarely make the promotional brochures.
Disadvantage 1: The Astronomical Cost Barrier (Beyond Just Purchase)
When discussing the Disadvantages of Medical Robots, cost is often the first hurdle mentioned, but its depth is frequently underestimated. The initial purchase price of a system like the da Vinci Surgical System – often exceeding $2 million – is merely the tip of the iceberg. Significant hidden costs rapidly accumulate:
Maintenance Contracts: These are non-negotiable and can run into hundreds of thousands of dollars annually. Failure to maintain the contract often voids warranties and halts access to critical software updates. Specialized Consumables: Proprietary instruments and accessories, required for each procedure, add thousands per surgery. These instruments have a limited number of uses before requiring expensive replacement. Infrastructure Upgrades: Operating rooms often need structural modifications, specialized tables, and enhanced electrical/data systems to accommodate the robots. Training Investment: Surgeons and support staff require extensive, ongoing training, taking them away from clinical duties and incurring substantial costs. A 2020 study in JAMA Surgery highlighted that the total cost of robotic surgery programs often exceeds initial projections by 30-50% when factoring in these hidden elements, raising serious questions about cost-effectiveness compared to traditional laparoscopic or open techniques for many common procedures.
The Medical Robotics Revolution: How da Vinci Became the World's Most Famous Surgical Assistant
Disadvantage 2: The Illusion of Autonomy & The Critical Human Factor
A common misconception fueled by media portrayals is that medical robots operate independently. In reality, current surgical robots are sophisticated telemanipulators. Every movement of the robotic arm is directly controlled by a human surgeon seated at a console. This introduces significant human-dependent Disadvantages of Medical Robots:
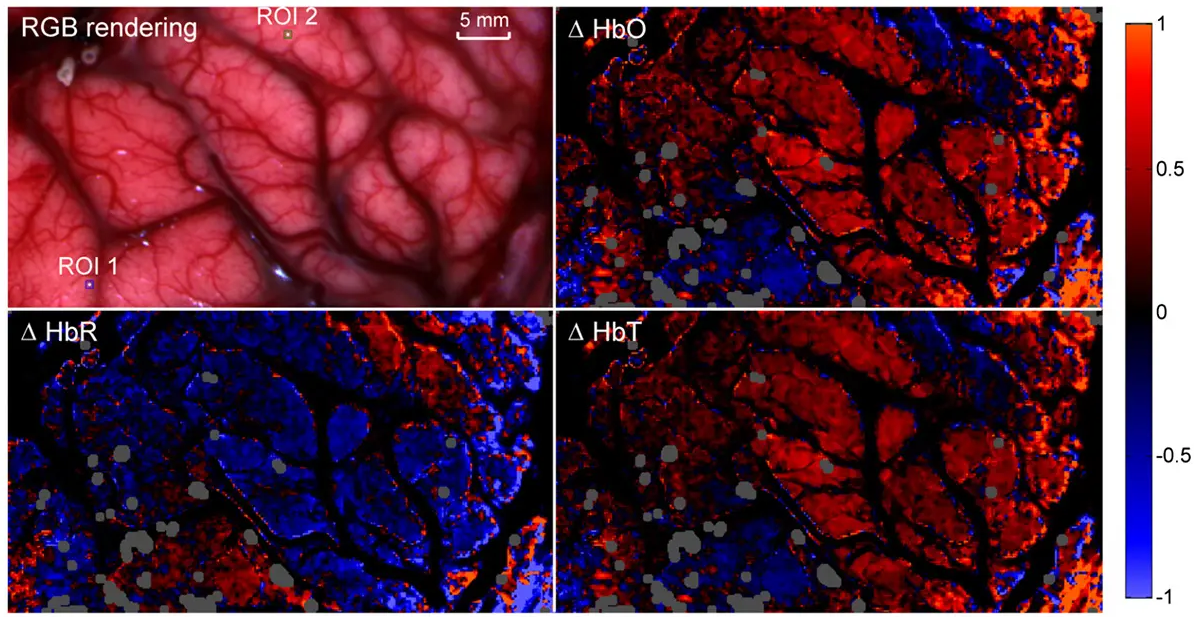
Learning Curve & Skill Variability: Mastering robotic surgery requires a different skill set than traditional methods. Proficiency varies greatly between surgeons, and the learning curve can be steep, potentially impacting patient outcomes during the initial adoption phase. Studies show complication rates can be higher for surgeons early in their robotic training. Loss of Tactile Feedback (Haptics): A major limitation is the near-total loss of tactile sensation. Surgeons rely heavily on visual cues on a screen, missing the subtle "feel" of tissue that guides decisions in open or laparoscopic surgery. This can increase the risk of inadvertent tissue damage, like applying too much force to a suture or misjudging the strength of a structure. Surgeon Fatigue & Ergonomics: While designed to be ergonomic, prolonged concentration in the console can lead to surgeon fatigue and physical strain, potentially impacting performance during lengthy procedures.
Disadvantage 3: Systemic Vulnerabilities and Unforeseen Complications
Integrating complex robotic systems into the intricate ecosystem of a hospital introduces unique vulnerabilities that constitute critical Disadvantages of Medical Robots:
Technical Failures & Downtime: Like any sophisticated machine, robots can malfunction. System errors, software glitches, or hardware failures mid-surgery can necessitate conversion to an open procedure, increasing patient risk and operative time. Scheduled and unscheduled downtime for maintenance or repairs can disrupt surgical schedules significantly. Cybersecurity Risks: Network-connected robots represent potential entry points for cyberattacks. Malicious actors could theoretically disrupt systems, steal sensitive patient data, or even attempt to manipulate device functions, posing unprecedented safety threats. While manufacturers implement safeguards, the risk profile is inherently higher than for non-connected surgical tools. Limited Versatility: Despite marketing, most current systems excel in specific procedures (e.g., prostatectomy, hysterectomy) but are less adaptable or efficient for others. Hospitals face pressure to utilize their expensive investment, potentially leading to its use in cases where simpler, cheaper methods might be equally or more effective.
Reporting Gaps: Concerns exist regarding the under-reporting of adverse events and malfunctions related to robotic surgery. A Johns Hopkins analysis suggested that incidents might be significantly underreported to the FDA compared to other medical devices, making a comprehensive understanding of risks challenging.
Frequently Asked Questions (FAQs)
A: Several factors drive adoption: market competition (hospitals feel pressure to offer "cutting-edge" tech), patient demand fueled by marketing, potential for improved outcomes in *specific* complex procedures, and surgeon preference. However, robust evidence proving *overall* cost-effectiveness across the board remains limited, highlighting a key tension within the Disadvantages of Medical Robots debate.
A: Liability is complex and evolving. It can potentially involve the surgeon (for errors in controlling the system), the hospital (for maintenance or training failures), and the manufacturer (for design flaws or software bugs). Determining fault often requires intricate investigation, making this a significant legal and ethical concern surrounding robotic surgery.
A: Current technology is nowhere near full autonomy for complex surgery. Robots are tools augmenting a surgeon's skills, not replacing their judgment, decision-making, and dexterity. While AI may play a larger role in diagnostics and planning, the intricate, adaptive, and often unpredictable nature of surgery makes complete replacement unlikely in the foreseeable future. The focus should be on collaboration, not replacement.
A: The safety profile is nuanced. For specific, well-defined procedures performed by highly experienced surgeons, robotic systems can offer advantages like enhanced visualization and precision in confined spaces, potentially reducing certain complications (like blood loss). However, the loss of haptic feedback, the learning curve, and the risk of technical failures introduce *different* risks. Large-scale, long-term studies comparing outcomes across a broad range of procedures and surgeon experience levels are still needed to definitively claim superior overall safety.
Conclusion: A Balanced View of Robotic Medicine
Medical robots represent a remarkable technological advancement with demonstrable benefits in specific surgical domains. However, uncritical enthusiasm obscures the significant Disadvantages of Medical Robots. The astronomical total cost of ownership, the critical dependence on human skill coupled with the loss of tactile sensation, and the systemic vulnerabilities introduced by complex technology demand careful consideration. Understanding these drawbacks is not about rejecting innovation, but about fostering realistic expectations, ensuring appropriate use, demanding rigorous cost-benefit analyses, and prioritizing patient safety above all else. The future of robotic medicine lies not in blind adoption, but in thoughtful integration that acknowledges both its potential and its profound limitations.