Imagine an operation where incisions are no larger than a keyhole, but a surgeon’s movements—scaled, steadied, and translated through miniature robotic arms working deep inside your body—achieve superhuman precision. This is the promise of medical robotics. But behind the glowing headlines of "surgical breakthroughs" lies a complex story of breathtaking capabilities intertwined with significant hurdles. This isn't just about cool tech; it’s about understanding how robots reshape healthcare's reality. We cut through the hype to deliver an unvarnished exploration of the very real Advantages And Disadvantages Of Medical Robots, dissecting their impact on surgeries, diagnostics, patient care, and the future of medicine. Knowing these pros and cons is crucial for patients, practitioners, and policymakers navigating this robotic revolution.
The Power of Precision: Unpacking the Advantages Of Medical Robots
Medical robots represent a paradigm shift in healthcare delivery, offering capabilities far exceeding traditional methods. These benefits are driving their adoption despite the costs and challenges.
Enhanced Surgical Precision & Minimally Invasive Excellence
The most lauded benefit is unprecedented surgical precision. Systems like the da Vinci Surgical System filter out natural hand tremors (The Medical Robotics Revolution: How da Vinci Became the World's Most Famous Surgical Assistant) and allow surgeons to scale down their movements (e.g., a 5:1 scale), enabling operations on structures millimeters wide through ports often smaller than 1cm. This dramatically reduces unintentional tissue damage. Consequently, complex procedures—prostatectomies, hysterectomies, intricate cancer resections—can now be performed minimally invasively (laparoscopically) when they previously required large, debilitating open incisions. This directly translates to reduced blood loss during surgery.
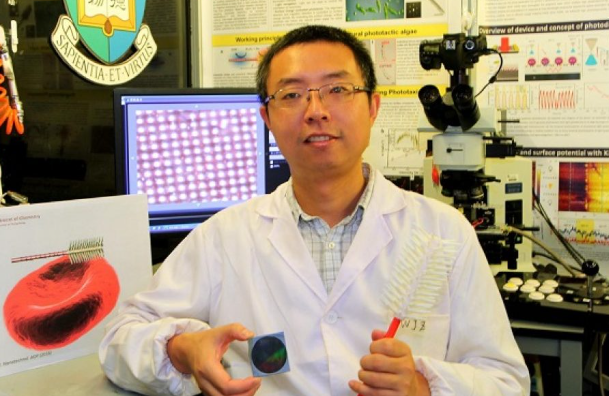
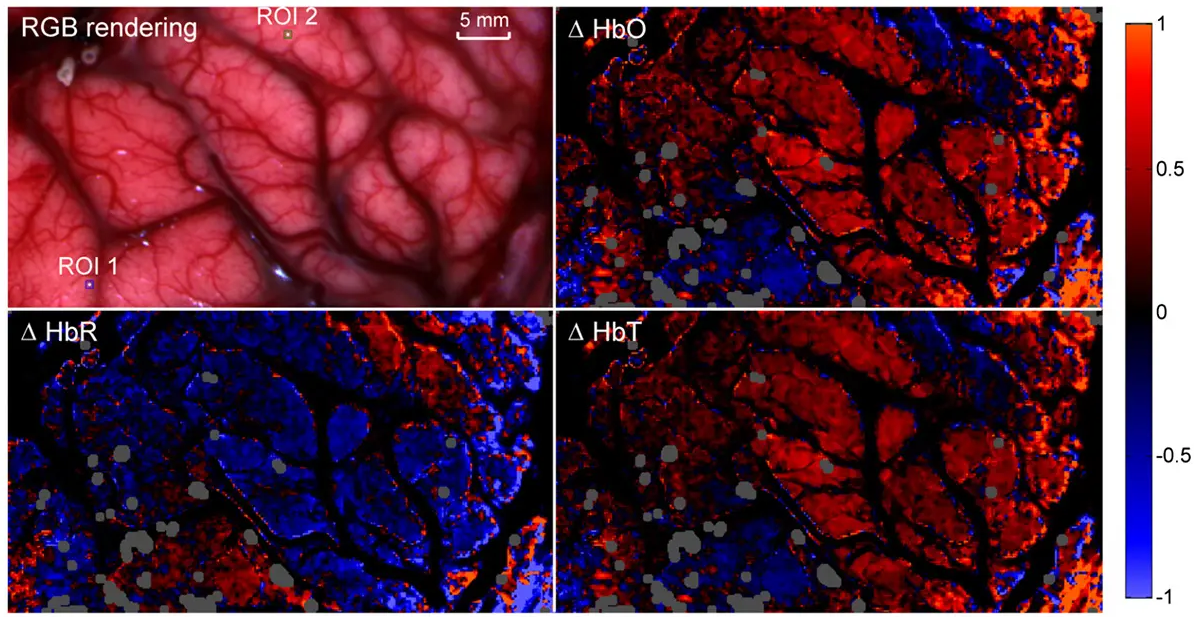
Superior Visualization & Dexterity Beyond Human Limits
Robotic surgery platforms incorporate high-definition, magnified (often 10x or greater) 3D visualization systems. Surgeons operate not by looking directly at the patient, but through a console providing an immersive, illuminated, and magnified view deep inside the operative field, far surpassing traditional laparoscopy. Furthermore, the robotic wrists possess a full range of motion (articulating at the instrument tip), mimicking the human wrist but with greater degrees of freedom. This "EndoWrist" technology allows access to confined anatomical spaces and complex maneuvers like suturing in tight corners with greater ease.
Improved Clinical Outcomes & Patient Recovery Metrics
Compelling clinical evidence links robotic assistance to tangible patient benefits. Studies across various procedures consistently report:
Significantly Reduced Hospital Stays: Major robotic prostatectomy patients often leave in 1-2 days vs. 3-5+ for open surgery.
Lower Complication Rates: Reduced risk of surgical site infections and other perioperative complications.
Decreased Postoperative Pain: Smaller incisions and less tissue trauma lead to lower pain scores and reduced opioid requirements.
Faster Return to Daily Activities: Patients resume work and normal life much quicker.
Potentially Better Functional Outcomes: Critical in areas like nerve-sparing during prostate cancer surgery impacting urinary continence and sexual function.
Expanded Accessibility & Standardization in Complex Procedures
Robotic systems enable surgeons to perform highly complex minimally invasive procedures that were previously either impossible laparoscopically or required extreme expertise honed over years. This effectively democratizes access to minimally invasive techniques for challenging cancers or reconstructive surgeries across more hospitals and regions. Moreover, the technology promotes standardization. Complex steps, viewed consistently through high-quality imaging and executed with precise instruments, can be performed more uniformly, reducing performance variability between surgeons.
Beyond the Hype: Confronting the Disadvantages Of Medical Robots
While transformative, medical robotics is not without substantial drawbacks. Acknowledging these challenges is vital for responsible integration into healthcare systems.
Staggering Acquisition & Operational Costs
The most immediate barrier is financial. A single new da Vinci Surgical System can cost between $1-$2.5 million. Beyond this massive capital expense are substantial recurring costs: proprietary, often single-use instruments costing hundreds to thousands per procedure ($700-$3000+ per case), annual service contracts exceeding $100,000, and specialized training. This creates a significant burden for hospitals, potentially limiting deployment, especially in resource-constrained settings or developing countries. The high costs inevitably contribute to rising healthcare expenditures.
The Steep & Demanding Learning Curve
Mastery of robotic surgery requires extensive, dedicated training that differs significantly from traditional or laparoscopic surgery. Surgeons must learn new psychomotor skills: operating via a console translating 2D hand movements into 3D instrument actions, mastering camera control with foot pedals, and adapting to the lack of tactile feedback (a critical limitation). Achieving proficiency often requires dozens of supervised procedures, involving substantial time investment and potentially impacting operating room efficiency during the learning phase.
Loss of Haptic Feedback & Integration Limitations
Current surgical robots lack genuine haptic (tissue feel) feedback. Surgeons rely entirely on visual cues – seeing tissue deformation or suture tension – to infer tactile sensations. This requires significant adaptation and can pose risks, like applying excessive force on delicate tissues or inadvertently breaking sutures. Furthermore, while advanced in their niche, many robotic systems operate as somewhat isolated platforms, lacking seamless integration with other hospital IT systems (Electronic Health Records, imaging archives) or newer real-time intraoperative guidance technologies.
Ethical & Accessibility Dilemmas
The immense cost raises serious ethical concerns about equitable access. Do only affluent patients or institutions in wealthy regions deserve the benefits of robotic precision? Can systems justify their cost based on incremental outcomes over proven, less expensive techniques for certain procedures? There’s also the potential for overuse driven by marketing pressure, patient demand influenced by perceptions of "better" technology, and revenue generation needs for hospitals seeking to recoup their investment. These factors could lead to inappropriate robotic surgeries.
Vulnerability & Systemic Risks
Medical robots, like any networked medical device, are potential cybersecurity targets. A breach could disrupt surgeries, compromise sensitive patient data processed by the system, or even lead to physical manipulation risks (though considered highly complex to execute). Dependence on a single system can also create bottlenecks; if the robot malfunctions, elective procedures relying on it may be canceled or require conversion to traditional techniques. Malfunctions, while rare, carry high stakes during active surgery.
Beyond Surgery: Exploring Advantages And Disadvantages Of Medical Robots Across Healthcare
The robotic revolution extends far beyond the operating room. Let's explore pros and cons in other critical domains:
Diagnostics & Imaging Robots
Advantages:
Increased Repetition & Throughput: Robotic arms in labs can handle samples 24/7 with consistent accuracy.
Enhanced Accuracy: Automated pipetting reduces human error in complex diagnostic workflows.
Early Detection Power: AI-integrated imaging robots (e.g., for radiology) can flag subtle anomalies potentially missed by the human eye.
Remote Diagnostics: Robotic telepresence allows specialists to consult or guide exams remotely.
Disadvantages:
High Setup Costs: Automated labs require significant capital investment.
AI Interpretation Uncertainty: Over-reliance on AI findings without robust human validation carries risks ("alert fatigue" or missed nuances).
Job Displacement Fears: Concerns over automation replacing certain lab technician roles.
Rehabilitation & Care Robots
Advantages:
Consistent, Quantifiable Therapy: Robotic exoskeletons or limbs offer highly repetitive, measurable movement therapy crucial for neuro-recovery.
Improved Caregiver Support: Lift assist robots reduce caregiver strain and patient injury risk during transfers.
Patient Independence: Robotic mobility aids or prosthetics enhance independence for individuals with disabilities.
Companionship Potential: Social robots combat loneliness in elderly care settings.
Disadvantages:
Affordability & Access: Cutting-edge rehab robotics remain prohibitively expensive for many.
Human Touch Deprivation: Overuse risks reducing essential human contact crucial for emotional well-being in care settings.
Complexity & Training: Require significant user/caregiver training and ongoing technical support.
Psychological Barriers: Some patients may resist or feel uncomfortable interacting with care robots.
The Human Element Impact: Workforce Transformation
Understanding Advantages And Disadvantages Of Medical Robots necessitates examining their profound effect on the healthcare workforce:
Upskilling & Role Evolution
Robotic surgery has created new specialized roles (e.g., robotic surgical first assistants) and required existing staff (scrub nurses, surgical techs) to master complex instrumentation setup and troubleshooting. This drives specialized skill acquisition and potentially higher earning potential for those who adapt.
The Reskilling Imperative & Job Displacement Concerns
Simultaneously, tasks previously performed by humans (like repetitive lab analysis or certain aspects of physical therapy guidance) may become automated. While new jobs emerge, the transition requires proactive workforce planning, substantial reskilling programs, and ethical management to mitigate potential displacement in specific sectors like medical labs.
The integration of medical robots demands careful planning to ensure healthcare professionals are equipped for evolving roles and new technologies like those shaping Leading AI. Ongoing education and adaptation are key.
Navigating the Robotic Future: Key Questions Answered (FAQs)
Q: Are robotic surgeries actually safer than traditional or laparoscopic surgeries?
A: Safety profiles vary by procedure and surgeon expertise. While robots offer distinct advantages like tremor reduction and enhanced visualization, leading to potentially reduced complications (less blood loss, fewer infections), they are tools. Surgeon skill and case selection remain paramount. Studies generally show robotic surgery is comparable or has specific advantages for complex minimally invasive cases, but may not be safer for every single procedure type. Reporting of adverse events specific to the robotic system is also continually evolving.
Q: Can a surgical robot ever truly "replace" a surgeon?
A: Not in the foreseeable future, and likely never completely. Current robots are master-slave systems. The surgeon is in complete control at the console; the robot has no autonomy. It simply translates the surgeon’s hand movements with enhancements. While AI is being integrated for assistance (like suggesting anatomy identification), complex surgical decision-making, handling unexpected complications, ethical judgment, and patient communication profoundly require human cognition, experience, and empathy. Robots augment surgeons; they do not replace them.
Q: What's the biggest ethical concern beyond cost related to medical robots?
A: Equitable access and potential overuse driven by non-clinical factors stand as major ethical issues. Ensuring that life-enhancing or life-saving robotic technology isn't solely available to privileged populations is a societal challenge. Simultaneously, the powerful marketing of these technologies, coupled with patient demand for perceived "high-tech" care, and the financial pressures on hospitals to utilize expensive equipment, could lead to procedures being performed robotically without clear evidence of significant benefit over safer, cheaper alternatives for that specific case. Maintaining patient-centered, evidence-based practice is crucial.
Q: What’s the next major frontier for medical robotics?
A: The convergence is key:
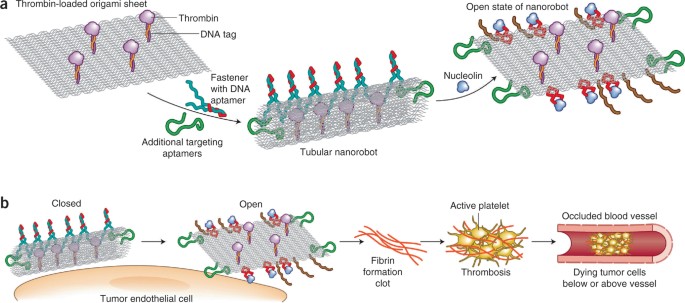
Enhanced AI Integration: Moving beyond navigation assistance to predictive analytics (predicting tissue response, optimizing surgical paths) and adaptive automation of routine subtasks under surgeon supervision.
Micro and Nanorobotics: Developing tiny robots for targeted drug delivery, micro-surgery within blood vessels, or minimally invasive diagnostics at a cellular level.
Haptic Feedback Solutions: Research into reliable ways to provide surgeons with realistic touch sensations remains a high priority.
Telerobotics for Extreme Distances: Expanding reliable remote surgical capabilities for regions lacking specialists.
The Human-Machine Synergy in Healthcare
The exploration of Advantages And Disadvantages Of Medical Robots reveals a fascinating tension between technological marvel and practical reality. The Advantages – unparalleled precision, minimally invasive triumphs, improved outcomes, and democratization of complex techniques – are profoundly impactful, saving lives and improving recovery for countless patients. Yet, the Disadvantages – staggering costs, a demanding learning curve, inherent technical limitations like the loss of touch, deep ethical quandaries, and systemic risks – are significant hurdles that cannot be glossed over.
Medical robots are not a panacea. They are powerful tools demanding thoughtful integration. Their ultimate value lies not in replacing the surgeon, but in augmenting human skill. The surgeon's judgment, experience, dexterity, and empathy, combined with the robot's steadiness, vision, and access, create a synergy greater than the sum of its parts. Navigating this future requires balancing technological optimism with pragmatic assessment. It demands prioritizing patient benefit above all, ensuring equitable access, investing in robust training and ethical frameworks, and continuously evaluating where robotic intervention offers genuine value over established methods.
As AI advances and robotics become more sophisticated and potentially affordable, this synergy will deepen. Understanding both the immense potential and the substantial challenges outlined in this analysis is the first step towards harnessing the power of medical robots responsibly, shaping a future where technology truly serves to enhance the human capacity to heal and care.