Imagine an operating room where surgeons operate with superhuman precision through incisions smaller than a dime, guided by 3D vision that sees through tissue. This isn’t science fiction—it’s the reality of modern surgical robots. These technological marvels transform complex procedures into minimally invasive feats, reducing human tremor by filtering hand movements into micro-scale actions while providing unprecedented visual access to surgical sites. They're not replacing surgeons; they're augmenting human capability beyond biological limits. This article pulls back the surgical curtain to reveal how these machines actually function beside flesh-and-blood medical teams, turning previously impossible operations into routine success stories.
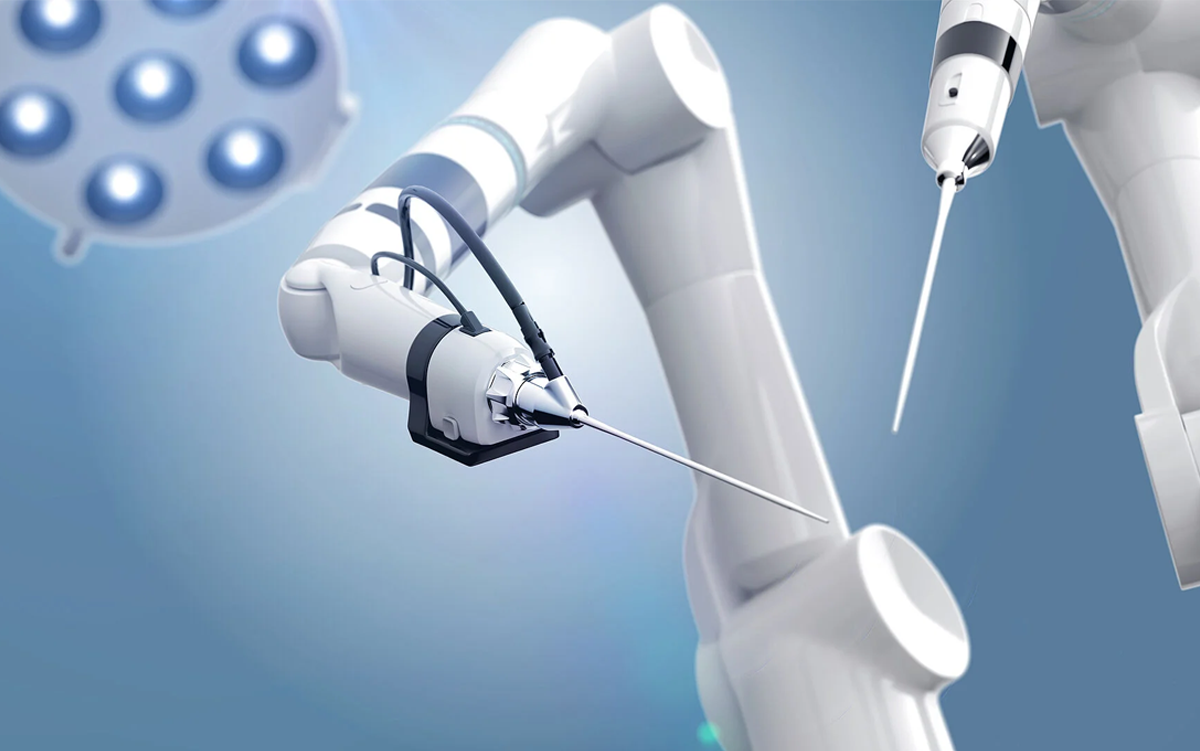
Robotic Arms: The Surgeon's Physical Proxies
Medical robots translate a surgeon's hand movements at the console into microscopically precise actions through wristed instruments that rotate 360°. Unlike rigid laparoscopic tools, these robotic arms bend like human wrists, enabling complex maneuvers in confined spaces like the pelvis or chest cavity. Each tremor gets filtered algorithmically—research shows tremor reduction of up to 80% compared to manual techniques. This facilitates suturing blood vessels narrower than 2mm in cardiac surgery, previously considered too risky for traditional methods.
Digital Vision Systems: Seeing the Unseeable
High-definition 3D cameras embedded in robotic systems offer 10x magnification of the surgical field, revealing microscopic structures invisible to the naked eye. Specialized imaging modes like fluorescence guidance highlight tumor margins using injected dyes, letting surgeons see cancer cells light up during resection. A recent Harvard Medical School study demonstrated how this technology cut positive margin rates by 52% in prostatectomies, dramatically reducing recurrence rates while preserving healthy tissue.
What Do Medical Robots Do Beyond Manual Tasks?
AI-Powered Decision Support During Critical Moments
Modern surgical platforms leverage intraoperative AI to analyze real-time tissue perfusion. During colorectal procedures, algorithms measure blood flow at anastomosis sites using hyperspectral imaging, predicting leak risks within seconds—data shows a reduction in anastomotic leaks of up to 60% with this technology. Meanwhile, neural networks cross-reference live anatomy with pre-op scans to flag deviations, like unexpected vascular structures near tumors.
Haptic Data Translation: The Missing Sensory Dimension
Unlike earlier generations, next-gen robots incorporate force feedback, converting tissue resistance into tactile sensations surgeons feel through console controllers. Johns Hopkins researchers quantified how this feature reduces suture breakage by translating nano-newton pressure levels—equivalent to the weight of a grain of rice—into actionable feedback during microsurgery.
Motion Analytics: Quantifying Surgical Skill
Robotic systems track movement efficiency metrics like path length and idle time. These analytics generate objective performance scores during training surgeries, shortening robotic surgery learning curves by an average of 14 cases according to a NEJM study. Such data is revolutionizing surgical credentialing beyond subjective assessment.
Da Vinci's Legacy: From Mechanics to Machine Learning
 The da Vinci system pioneered robotic surgery by introducing wristed instruments and 3D visualization decades ago. Now, its latest iterations feature proprietary machine learning that adapts to a surgeon's motor patterns, anticipating instrument positions and automating camera movements. A key advantage over new competitors is its robust interoperability with hospital EHRs and imaging systems—da Vinci holds over 1,200 patents covering these integrations. Intuitive Surgical reported 12% more procedures globally in 2023 compared to pre-pandemic volumes.
The da Vinci system pioneered robotic surgery by introducing wristed instruments and 3D visualization decades ago. Now, its latest iterations feature proprietary machine learning that adapts to a surgeon's motor patterns, anticipating instrument positions and automating camera movements. A key advantage over new competitors is its robust interoperability with hospital EHRs and imaging systems—da Vinci holds over 1,200 patents covering these integrations. Intuitive Surgical reported 12% more procedures globally in 2023 compared to pre-pandemic volumes.
The Medical Robotics Revolution: How da Vinci Became the World's Most Famous Surgical Assistant
Future Capabilities: What Surgeons Can't Do (Yet)
1Autonomous Suturing: Prototype systems at UC Berkeley finished suturing in pig bowel resections 40% faster than manual methods, using computer vision to place stitches at optimal tension—this could reduce 6-hour surgeries by 90 critical minutes.
2Biologic Welding: MIT's laser-guided robots seal incisions with thermal energy rather than sutures, creating scarless closures at cellular resolution—animal trials show 6x faster healing in intestinal repairs.
3Tumor-Hunting Nanobots: Magnetically-guided microbots under development at ETH Zurich can navigate bloodstreams to biopsy unreachable lesions, capturing cellular samples with microscopic forceps—a breakthrough for early pancreatic cancer diagnosis.
Common Myths Debunked: Separating Hollywood from Healthcare
| Myth | Reality |
|---|---|
| Robots operate autonomously | Every movement mirrors surgeon input at the console; systems have no decision-making capability |
| Robotic = fully automatic | "Robotic" refers to instrument control method—surgeons operate tools remotely with precision augmentation |
| All robotic surgery is the same | Platforms specialize—orthopedic robots sculpt bone (MAKO), while neurosurgical bots like ROSA work on sub-millimeter accuracy |
Medical Robotics FAQs
Q: What Do Medical Robots Do that human surgeons physically cannot?
A: They execute movements with 0.1mm precision (beyond human motor control), maintain stability for hours without fatigue, and operate through incisions too small for human hands while providing magnified 3D visualization deep inside cavities.
Q: How do robots handle surgical complications?
A: When unexpected bleeding occurs, systems like da Vinci offer integrated vessel sealing at console touchpoints. AI-powered systems can identify anomalous anatomy in real-time using comparative imaging and alert surgeons before critical errors occur.
Q: Do surgical robots actually improve patient outcomes?
A: According to JAMA meta-analysis, robotic surgery reduces complications in complex procedures—for instance, converting open surgeries to minimally invasive robotics cut infection rates by 68% and shortened hospital stays by 3.5 days.