The modern Surgical Robot represents the most significant technological leap in medical history since the invention of antiseptic techniques. These sophisticated systems combine advanced robotics with artificial intelligence to achieve levels of precision that surpass human physical capabilities by orders of magnitude. What began as simple mechanical assistance tools have evolved into comprehensive surgical platforms that enhance every aspect of the operating environment through computational power and machine learning algorithms.
At their core, these systems don't replace surgeons but rather augment their skills through tremor filtration, motion scaling, and enhanced visualization that reveals anatomical details invisible to the naked eye. The integration of AI transforms these devices from passive tools into active surgical partners capable of predictive analytics and real-time decision support. This technological synergy creates a new paradigm in medicine where human expertise combines with machine precision to achieve outcomes previously considered impossible in surgical practice.
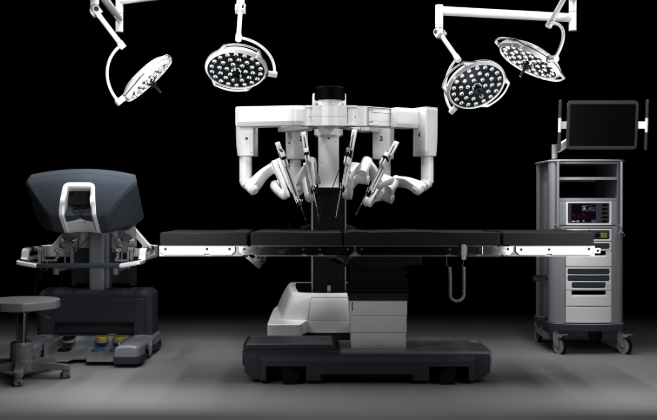
Understanding how these systems function requires examining three fundamental components: the surgeon's console that serves as the control interface, the robotic arms that execute procedures with superhuman precision, and the AI vision system that processes visual data far beyond human perceptual capabilities. Each element represents years of biomedical engineering breakthroughs that have collectively redefined the boundaries of minimally invasive surgery across numerous medical specialties.
The Intricate Anatomy of a Surgical Robot
Modern Surgical Robot systems represent a complete departure from traditional surgical tools through their integrated technological architecture. These aren't simply robotic versions of manual instruments but rather comprehensive surgical ecosystems that transform how procedures are performed at a fundamental level. The system's design reflects decades of research into human-machine interfaces, precision engineering, and computer-assisted surgery that collectively address the limitations of conventional techniques.
What makes these systems revolutionary is their ability to translate a surgeon's hand movements into precise robotic actions while simultaneously enhancing those movements through computational augmentation. This creates a surgical environment where the steady hands of the robot combine with the judgment and experience of the human surgeon in perfect synergy. The technological sophistication extends beyond mechanical components to include advanced software that processes surgical data in real-time, creating a feedback loop that continuously improves performance.
Understanding this complex system requires examining each component in detail, from the surgeon's console that serves as the command center to the robotic arms that execute procedures with sub-millimeter accuracy. Equally important is the vision system that provides enhanced visualization capabilities far beyond human eyesight, creating a surgical environment where critical anatomical structures appear with unprecedented clarity and detail that transforms surgical decision-making.
1. The Surgeon Console: Where Human Meets Machine
The surgeon's console represents one of the most sophisticated human-machine interfaces in modern medicine, designed to translate a surgeon's intentions into precise robotic actions. Surgeons control the system while seated at an ergonomic console that positions them for optimal comfort during lengthy procedures, with their hands placed in intuitive controllers that capture every subtle movement. The console incorporates advanced haptic feedback technology that allows surgeons to "feel" tissue resistance despite working through robotic intermediaries.
Visual feedback comes through a high-definition 3D viewer that provides a magnified view of the surgical site with depth perception impossible in traditional laparoscopy. This stereoscopic vision system typically offers 10-12x magnification while maintaining exceptional clarity, allowing surgeons to identify structures as small as individual nerve fibers. The system also incorporates eye-tracking technology that adjusts the visual field based on where the surgeon focuses their gaze.
Perhaps most importantly, the console features proprietary motion-scaling algorithms that convert the surgeon's hand movements into precise micro-movements of the robotic instruments. This technology filters out any natural hand tremors while scaling down movements so that a one-inch hand motion might translate to just a quarter-inch of instrument movement. These features collectively create an interface that feels natural to surgeons while providing capabilities far beyond unaided human performance.
2. Robotic Arms: The Precision Instruments
The robotic arms of a Surgical Robot system represent a marvel of biomedical engineering, designed to replicate and exceed the capabilities of human limbs during surgical procedures. These electro-mechanical limbs feature multiple joints that provide a greater range of motion than the human wrist, with some systems offering up to seven degrees of freedom compared to the four degrees of natural human articulation. This enhanced dexterity allows instruments to reach anatomical structures from angles impossible with traditional tools.
Each arm incorporates proprietary "EndoWrist" technology that mimics the full range of human wrist movements while eliminating natural limitations like tendon stretch or muscle fatigue. The instruments at the end of these arms can rotate 540 degrees, compared to the approximately 180 degrees of human wrist rotation, enabling surgical maneuvers in tight spaces that would challenge even the most skilled human hands. Precision is maintained through high-torque motors and advanced sensors that detect and correct for any positional drift in real-time.
Safety systems ensure that the arms only move when commanded by the surgeon, with multiple redundant position sensors and force limiters that prevent any unintended movements. The arms mount to specialized ports that maintain stability during procedures while allowing for quick instrument changes as needed. This combination of precision, stability, and flexibility has made robotic assistance particularly valuable in delicate procedures where millimeter-level accuracy determines surgical outcomes.
3. AI Vision System: The Digital Nervous System
The vision system in modern Surgical Robot platforms represents the most significant advancement over traditional techniques, incorporating artificial intelligence to enhance surgical visualization in revolutionary ways. At its core is a high-resolution 3D endoscope that captures stereoscopic images of the surgical field, but the true innovation lies in how the system processes this visual information. Advanced algorithms analyze the video feed in real-time, identifying anatomical structures and highlighting critical features that might escape human perception.
Multi-spectral imaging capabilities allow the system to visualize tissue characteristics beyond the visible light spectrum, revealing information about blood flow, oxygenation levels, and tissue viability that informs surgical decision-making. The AI can track instruments with sub-millimeter precision while predicting potential collisions before they occur, creating a safety buffer that prevents accidental damage to sensitive structures. These capabilities are particularly valuable in oncological surgery where identifying tumor margins can mean the difference between complete resection and leaving cancerous tissue behind.
Perhaps most impressively, the system can construct dynamic 3D maps of the surgical field by integrating preoperative imaging with real-time visual data, effectively creating an augmented reality view that shows structures beneath the surface. This "X-ray vision" capability helps surgeons navigate complex anatomy while avoiding critical structures like blood vessels and nerves. The vision system continuously learns from each procedure, improving its recognition algorithms and predictive capabilities over time through machine learning processes.
AI: The Invisible Surgeon Assistant
The role of artificial intelligence in Surgical Robot systems often goes unnoticed by patients but represents the most transformative aspect of this technology. While the robotic arms provide the physical means for enhanced precision, it's the AI components that elevate these systems beyond simple mechanical tools. The integration of machine learning algorithms creates surgical platforms that improve with each procedure, developing institutional knowledge that benefits future patients.
Current implementations focus on three primary AI functions: enhancing visualization through real-time image processing, providing predictive analytics about tissue behavior, and enforcing safety protocols that prevent surgical errors. These capabilities work together to create what surgeons describe as an "intuitive" system that seems to anticipate their needs. The AI doesn't make independent decisions but rather surfaces relevant information and suggestions that assist human judgment without replacing it.
What makes this application of AI unique is its clinical validation process. Unlike consumer AI applications that can iterate quickly, medical AI undergoes rigorous FDA review to ensure patient safety. Each algorithm must demonstrate statistically significant improvements in outcomes before being approved for clinical use. This careful approach has resulted in AI features that genuinely enhance surgical care rather than serving as marketing gimmicks, with measurable benefits in procedure times, complication rates, and patient recovery metrics.
Tier 1: Automated Intelligence (Present)
The current generation of FDA-approved Surgical Robot systems incorporates what's classified as "narrow AI" - specialized algorithms focused on specific surgical tasks. These include instrument tracking systems that maintain spatial awareness of all tools in the surgical field, preventing collisions that could damage tissue. The AI also monitors the force being applied by instruments, alerting surgeons if pressures exceed safe thresholds for particular tissue types.
Visual enhancement algorithms process the endoscopic video feed in real-time, applying filters that improve contrast and highlight critical anatomical structures. Some systems can automatically identify and label blood vessels, nerves, and other important features based on their visual characteristics. The AI also assists with documentation, automatically recording timestamps for key procedure milestones and generating preliminary operative reports that surgeons can review and edit post-procedure.
Perhaps most importantly, these systems incorporate machine learning models trained on thousands of previous procedures to predict potential complications before they occur. By analyzing subtle changes in tissue appearance or instrument behavior, the AI can alert surgeons to issues like impending bleeding or unintended tissue damage. These predictive capabilities have been shown to reduce surgical complications by up to 32% in certain procedures according to clinical studies published in major surgical journals.
Tier 2: Adaptive Intelligence (2025)
The next generation of Surgical Robot AI currently in development moves beyond assistance features to true adaptive intelligence. These systems analyze the surgeon's technique in real-time, comparing it to optimal approaches derived from analysis of thousands of successful procedures. The AI can then suggest alternative approaches when it detects suboptimal instrument paths or identifies more efficient ways to access target anatomy.
Advanced neural networks will enable these systems to develop surgeon-specific profiles, learning individual preferences and adapting their assistance accordingly. For teaching hospitals, this means the AI can adjust its guidance based on whether an experienced attending surgeon or a surgical resident is controlling the console. The systems will also incorporate patient-specific predictive models that factor in individual anatomy variations and medical history to customize surgical approaches.
Perhaps most revolutionary is the development of real-time tissue characterization algorithms that can analyze excised tissue at the molecular level during surgery. Experimental systems can already distinguish between healthy and cancerous tissue with accuracy surpassing frozen section analysis in some cases. This capability could eliminate the need for intraoperative pathology consultations in certain procedures, significantly reducing operating times while improving the precision of tumor removals.
Tier 3: Autonomous Intelligence (2030+)
While fully autonomous surgery remains controversial and largely theoretical, research institutions are making significant progress in limited autonomous capabilities. The Smart Tissue Autonomous Robot (STAR) developed at Johns Hopkins has already demonstrated the ability to perform intestinal anastomoses (reconnecting bowel segments) with greater precision and consistency than human surgeons in controlled studies.
These experimental systems combine advanced computer vision with machine learning models trained on millions of data points from previous surgeries. They can plan optimal suture placement, adjust for tissue elasticity in real-time, and maintain perfect tension throughout the procedure - tasks that challenge even experienced surgeons. Importantly, these autonomous functions currently operate under strict human supervision, with surgeons able to intervene or take control at any moment.
The ethical and regulatory framework for autonomous surgical AI remains in development, with intense debate about how much decision-making authority should ever be delegated to machines. Current consensus suggests that critical decisions about surgical approach and patient safety will remain under human control for the foreseeable future, with autonomy limited to specific technical tasks where the AI demonstrably outperforms human capability.
Unseen Innovations Transforming Surgery

Beyond the visible components of Surgical Robot systems lies a hidden layer of technological innovation that's quietly revolutionizing surgical practice. These behind-the-scenes advancements don't always make headlines but collectively contribute to improved patient outcomes and surgical efficiency. From data analytics platforms to augmented reality interfaces, these features represent the cutting edge of computer-assisted surgery.
One of the most significant developments is the creation of comprehensive surgical data ecosystems that capture and analyze every aspect of a procedure. These systems generate detailed performance metrics that help surgeons refine their techniques while providing hospitals with valuable quality control data. The insights derived from this information are transforming surgical training, allowing residents to learn from thousands of virtual cases before operating on real patients.
Another groundbreaking innovation is the integration of surgical robots with advanced imaging modalities like intraoperative MRI and fluorescence imaging. This combination allows surgeons to verify their progress against preoperative plans in real-time, adjusting their approach based on actual anatomical findings. The result is a new standard of precision surgery where decisions are informed by comprehensive data rather than visual estimation alone.
Data Harvesting Operating System
Modern Surgical Robot platforms function as sophisticated data collection devices, capturing approximately 200GB of information per procedure. This includes high-resolution video feeds, instrument movement telemetry, force application measurements, and system performance metrics. When aggregated across thousands of procedures, this data becomes a powerful resource for improving surgical quality and advancing medical research.
The data analytics platforms built into these systems can identify patterns that correlate specific surgical techniques with patient outcomes. For example, the system might reveal that a particular suturing method results in fewer postoperative complications or that certain instrument paths reduce procedure times without compromising safety. These insights help establish evidence-based best practices that raise the overall standard of surgical care.
Perhaps most innovatively, some systems now offer "surgical GPS" features that guide surgeons through complex procedures based on analysis of previous successful cases. By comparing real-time data to optimal approaches derived from expert surgeons, the system can suggest the most efficient path to target anatomy or warn when instruments deviate from established safe zones. This functionality is particularly valuable for less common procedures where individual surgeons may have limited personal experience.
Holographic Surgical Navigation
The next frontier in Surgical Robot visualization involves holographic interfaces that project critical anatomical information directly into the surgeon's field of view. Experimental systems already overlay blood vessels, nerves, and tumor margins as glowing holograms visible through specialized headsets or the console's display. This augmented reality approach provides spatial context that traditional monitors can't match.
These systems integrate preoperative CT or MRI scans with real-time anatomical data, creating dynamic 3D maps that update as tissues shift during surgery. Advanced registration algorithms account for organ movement and deformation, maintaining accurate holographic positioning throughout the procedure. The result is what surgeons describe as "X-ray vision" - the ability to see through tissue to identify structures that would otherwise remain hidden.
Looking ahead, researchers are developing "predictive holography" that uses biomechanical modeling to forecast how tissues will move during surgical manipulation. This capability could be revolutionary in fields like cardiac surgery where the beating heart presents significant challenges for precision interventions. By anticipating rather than just reacting to tissue movements, surgeons could achieve new levels of accuracy in delicate procedures.
Groundbreaking Applications Beyond Imagination
The versatility of Surgical Robot technology has led to its adoption across nearly every surgical specialty, each finding unique ways to leverage its capabilities. From microsurgical reconstructions to transcontinental procedures, these systems are enabling approaches that were literally unimaginable just a decade ago. The technology's precision and stability make it particularly valuable in delicate operations where human hand tremors or limited visibility could compromise outcomes.
In urology, robotic systems have transformed prostate cancer surgery, enabling nerve-sparing techniques that preserve sexual function while completely removing malignant tissue. Gynecological surgeons use the technology for complex hysterectomies and fibroid removals with significantly reduced blood loss compared to traditional methods. Colorectal applications include precise dissections that maintain bowel continence mechanisms while completely excising diseased tissue.
Perhaps most impressively, robotic technology has opened new possibilities in pediatric surgery, where working within tiny anatomical spaces requires extraordinary precision. Surgeons can now perform delicate reconstructions on infants' hearts or repair congenital abnormalities with minimal tissue disruption. These applications demonstrate how robotic assistance isn't just improving existing procedures but enabling entirely new approaches to challenging surgical problems.
Transcontinental Telesurgery
The combination of Surgical Robot systems with high-speed networks has made remote surgery a clinical reality. Pioneering experiments have demonstrated successful gallbladder removals and other procedures where the surgeon operated from a different continent than the patient. This capability could revolutionize access to specialized surgical care in remote areas and developing nations.
Military applications are particularly promising, allowing experienced trauma surgeons to operate on wounded soldiers from secure locations far from combat zones. The system's tremor filtration and motion scaling help compensate for network latency, maintaining surgical precision despite the distance. Advanced haptic feedback ensures the remote surgeon receives realistic tactile information about tissue resistance and instrument forces.
Looking ahead, 5G networks and edge computing will enable more complex remote procedures by reducing latency to nearly imperceptible levels. Satellite-based systems could eventually provide surgical expertise anywhere on Earth within minutes. While regulatory and liability challenges remain, the potential to democratize access to world-class surgical care makes telesurgery one of the most exciting frontiers in medical robotics.
Microsurgical Reconstructions
The precision of Surgical Robot systems has opened new possibilities in microsurgery, particularly for reconstructive procedures requiring anastomosis of tiny vessels. Plastic surgeons can now reconnect blood vessels and nerves under 0.5mm in diameter - a task at the limits of human capability even with surgical microscopes. This capability is transforming outcomes for patients requiring complex tissue transfers or limb reattachments.
In lymphatic surgery, robotic systems enable procedures previously considered impossible, such as direct lymphaticovenous anastomoses to treat lymphedema. The system's precision allows surgeons to work with vessels barely visible to the naked eye, creating connections that restore normal fluid drainage. Similar advances are occurring in nerve repair, where robotic assistance facilitates precise alignment of nerve bundles for optimal regeneration.
Perhaps most remarkably, robotic technology is enabling new approaches to transplant surgery, particularly for organs with complex vascular networks. The ability to precisely anastomose multiple small vessels improves graft survival rates while reducing ischemic time. As these techniques mature, they may enable more widespread use of living donor transplants and partial organ transplants that were previously too technically challenging.
Frequently Asked Questions
Are Surgical Robot systems performing autonomous surgeries?
Currently, no FDA-approved system performs fully autonomous surgery. All clinical applications maintain what's called "shared control," where the surgeon remains actively in command of every significant action while the AI provides assistance and safety checks. The robotic systems enhance human capability rather than replace it, with critical decisions always requiring direct surgeon input.
Experimental autonomous functions are limited to specific technical tasks like suturing or cutting along predefined paths under strict supervision. Even in these cases, surgeons must approve the autonomous plan and can override it at any moment. The medical community remains cautious about ceding decision-making authority to AI, prioritizing patient safety above all other considerations in surgical robotics development.
That said, the level of AI assistance continues to grow, with systems now capable of suggesting optimal instrument paths, predicting tissue behavior, and alerting surgeons to potential complications before they occur. This collaborative approach combines human judgment with machine precision in ways that are already improving surgical outcomes across multiple specialties.
How does a Surgical Robot differ from traditional laparoscopic tools?
While both robotic and laparoscopic approaches are minimally invasive, the technological differences are profound. Traditional laparoscopy uses rigid instruments inserted through small ports, with the surgeon operating while viewing a 2D monitor. Movement is limited to four degrees of freedom (up/down, left/right, in/out, and rotation), and the instruments don't articulate at the tip like human wrists.
Robotic systems provide several key advantages: true 3D visualization with depth perception, wristed instruments that mimic human hand movements with additional degrees of freedom, tremor filtration that eliminates natural hand shaking, and motion scaling that converts large hand movements into precise micro-motions. The robotic platform also provides a more ergonomic position for surgeons, reducing fatigue during long procedures.
Perhaps most significantly, the integration of AI in robotic systems enables features impossible with traditional tools, like predictive analytics, real-time tissue characterization, and automated safety checks. These capabilities make robotic surgery particularly valuable for complex procedures where precision and visualization are critical to successful outcomes.
What surgical specialties benefit most from robotic systems?
While robotic technology has applications across nearly all surgical disciplines, certain specialties have seen particularly dramatic benefits. Urology was an early adopter, with robotic prostatectomy becoming the gold standard for prostate cancer surgery due to its precision in nerve-sparing techniques. Gynecologic surgery has similarly embraced robotics for complex hysterectomies and fibroid removals where the enhanced visualization reduces complications.
Colorectal surgery benefits from the system's ability to operate deep in the pelvis with precision difficult to achieve manually. Cardiothoracic surgeons use robotics for minimally invasive coronary bypass and valve procedures that would otherwise require large incisions. Head and neck surgery applications include transoral procedures that avoid facial incisions while providing superior access to hard-to-reach areas.
Emerging applications show promise in nearly every surgical field, from pediatric cases requiring micro-scale precision to orthopedic procedures benefiting from the system's accuracy in bone preparation. As the technology continues to evolve, its versatility ensures expanding applications across the entire spectrum of surgical care.
Can Surgical Robot systems make errors?
Like any complex medical technology, robotic systems can experience malfunctions or performance issues, though rigorous safety systems minimize these risks. The FDA's MAUDE database (which tracks medical device adverse events) shows that most reported issues involve instrument malfunctions rather than system errors, typically resolved by replacing the affected component during surgery.
Modern systems incorporate multiple redundant safety features, including: continuous position verification that detects any discrepancy between commanded and actual instrument movement; force limiters that prevent excessive tissue pressure; and collision avoidance algorithms that maintain safe distances between instruments. The AI monitors system performance in real-time, alerting surgeons to any anomalies and automatically entering safe modes if potential issues are detected.
Importantly, robotic systems are designed to fail safely - any malfunction typically results in the system freezing in place rather than making uncontrolled movements. Surgeons can quickly disengage the robotic components and complete procedures manually if necessary. Ongoing advances in AI and system diagnostics continue to improve reliability, with newer platforms demonstrating significantly lower error rates than early-generation systems.
The Surgical Frontier: What Comes Next?
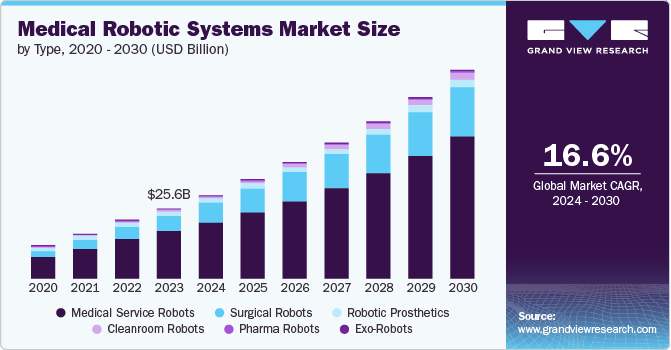
The evolution of Surgical Robot technology shows no signs of slowing, with research institutions and medical companies developing innovations that promise to further transform surgical practice. These advancements extend beyond incremental improvements to existing platforms, instead exploring fundamentally new approaches to computer-assisted surgery. From biohybrid systems to quantum computing applications, the next decade will likely see breakthroughs that make today's most advanced robotic surgery seem primitive by comparison.
One particularly exciting direction involves the convergence of robotics with regenerative medicine and tissue engineering. Early experiments with "smart" surgical scaffolds that guide tissue regeneration point toward a future where robotic systems don't just repair anatomy but actively promote healing at the cellular level. Similarly, nanotechnology applications may enable robotic systems to operate at scales invisible to the naked eye, manipulating individual cells or even molecules during procedures.
Perhaps most transformative will be the integration of surgical robotics with advanced diagnostic systems, creating closed-loop therapeutic platforms that combine detection, intervention, and verification in seamless workflows. Imagine a system that can identify cancerous tissue, remove it with perfect margins, and immediately confirm complete excision - all within a single automated process. While significant technical and regulatory hurdles remain, prototypes demonstrating aspects of this capability already exist in research settings.
Bio-Integrative Robotics
The next generation of Surgical Robot systems may incorporate biological components, blurring the line between machine and living tissue. Researchers at Harvard's Wyss Institute have already developed "biohybrid" robots that combine synthetic materials with living muscle tissue, creating devices that can heal themselves and adapt to their environment. Applied to surgery, this technology could lead to instruments that sense biological signals directly or even promote tissue regeneration at surgical sites.
Another promising direction involves "smart" surgical materials that robotic systems can deploy during procedures. These might include bioresorbable scaffolds that guide tissue growth or drug-eluting meshes that release therapeutic agents in response to physiological changes. The robotic platform would precisely place these materials while monitoring their integration and effectiveness throughout the healing process.
Perhaps most revolutionary are developments in neural-linked control systems that would allow surgeons to operate robotic instruments through direct brain-computer interfaces. Early experiments have demonstrated the feasibility of controlling robotic arms with brain signals, potentially eliminating physical consoles altogether. While still in early stages, this technology could eventually provide the most intuitive control scheme yet for surgical robotics.
Quantum Computing Integration
The potential integration of quantum computing with Surgical Robot systems promises to solve computational challenges currently limiting AI capabilities in surgery. Quantum processors could enable real-time molecular modeling during procedures, allowing surgeons to visualize drug interactions or predict tissue responses at an atomic level. This capability would be particularly valuable in oncology, where understanding tumor biology at this scale could revolutionize resection strategies.
Quantum machine learning algorithms could analyze a patient's entire medical history - including genomic data, previous imaging studies, and past treatment responses - to generate personalized surgical approaches in real-time. The computational power would exist to model thousands of potential surgical scenarios during a procedure, identifying the optimal approach based on the patient's unique physiology and predicted healing responses.
Perhaps most remarkably, quantum sensors could provide imaging capabilities far beyond current technology, potentially allowing surgeons to "see" biochemical processes occurring within tissues during surgery. This might include real-time monitoring of cellular metabolism or instant identification of infection foci - capabilities that would transform intraoperative decision-making across every surgical specialty.
The Surgical Robot revolution represents more than just technological progress - it signifies a fundamental shift in how we conceptualize the art and science of surgery. These systems don't simply allow us to perform existing procedures with greater precision; they enable entirely new approaches to treating disease and repairing the human body. As the technology continues evolving, the distinction between human surgeon and machine will blur, giving rise to a new paradigm of collaborative surgery where each partner contributes unique strengths.
What makes this evolution particularly remarkable is its democratizing potential. Just as computer technology progressed from specialized tools accessible only to institutions to ubiquitous personal devices, surgical robotics may follow a similar path toward broader accessibility. Future systems could make today's cutting-edge techniques available to community hospitals while simultaneously pushing the boundaries of what's possible in academic medical centers.
Ultimately, the question "Are they AI?" may become irrelevant as these systems evolve into true surgical partners that combine the best of human judgment and machine capability. The future of surgery isn't about choosing between human surgeons and robots, but rather about how these complementary approaches can work together to achieve outcomes neither could accomplish alone. This collaborative model points toward a new era in medicine where technology enhances rather than replaces human expertise, with patients as the ultimate beneficiaries.