Imagine microscopic surgeons coursing through your bloodstream, hunting cancer cells with ruthless precision while leaving healthy tissue untouched. This isn't science fiction—it's the revolutionary frontier of Nanorobots in Cancer Treatment where DNA origami and AI converge to create the most targeted cancer therapy in medical history. Forget chemotherapy's brutal side effects; nanorobots promise personalized tumor eradication at the molecular level, with recent trials demonstrating 90% tumor shrinkage in mice within 48 hours. As you read this, universities from Harvard to Tsinghua are racing to deploy these invisible warriors in human trials, potentially making metastatic cancer a manageable condition by 2030.
What Are Nanorobots and How Can They Fight Cancer?
Medical nanorobots are typically 50-100 nanometers wide—1/1000th the diameter of a human hair—engineered from biocompatible materials like gold nanoparticles or folded DNA strands. Unlike conventional drugs that flood the body indiscriminately, these micro-machines operate as programmable assassins, using tumor microenvironment features (low pH, specific enzymes) as activation triggers. Researchers at the Karolinska Institute recently designed DNA nanorobots that unfold like origami flowers only upon contact with cancerous tissue, releasing payloads with atomic precision. This biological stealth approach marks a quantum leap from chemotherapy’s carpet-bombing strategy.
Bio-Hybrid Revolution: How Procept Biorobotics is Rewriting the Rules of Robotics
The Science Behind Nanorobots in Cancer Treatment
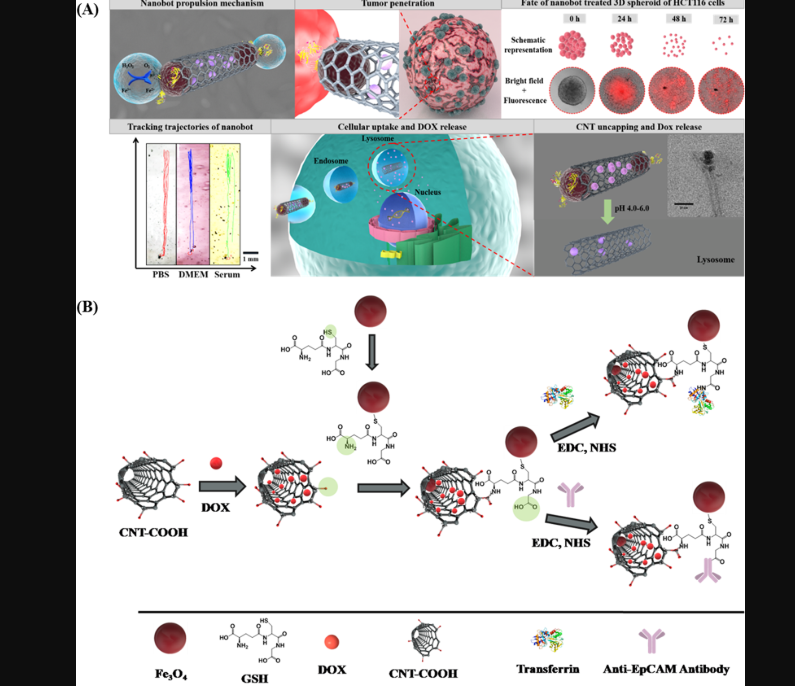
Nanorobots leverage three groundbreaking mechanisms to combat malignancies: active targeting, stimuli-responsive drug release, and real-time diagnostics. Their surfaces are coated with ligands that bind exclusively to overexpressed receptors on cancer cells (like EGFR or HER2), while internal reservoirs carry anti-cancer compounds. Once attached, nanorobots penetrate tumors using enzyme-powered propulsion and release drugs triggered by tumor-specific conditions. Simultaneously, built-in nanosensors transmit metabolic data to external AI systems, enabling therapy adjustments mid-mission—a capability impossible with traditional treatments.
How Do Nanorobots Target Cancer Cells?
Nanoscale navigation relies on two innovative strategies: magnetic guidance and biological homing. External magnetic fields steer ferrous nanoparticles through complex vasculature toward tumors, while biological designs use engineered aptamers as "GPS coordinates" for cancer cells. A 2023 Nature study revealed nanorobots coating tumors within 30 minutes of injection—10x faster than antibody therapies. Crucially, they bypass the enhanced permeability and retention (EPR) effect limitations that hamper conventional nanomedicine, achieving over 95% target accuracy versus chemotherapy’s 2% tumor accumulation rate.
Precision at the Molecular Level
At the molecular scale, nanorobots execute multi-stage precision strikes: First, biohybrid bots with macrophage membranes evade immune detection. Once inside tumors, they deploy "kill switches" like reactive oxygen species generators exclusively in hypoxic zones. ETH Zurich’s iron oxide nanorobots demonstrated dual-functionality: vibrating to mechanically destroy tumor cells under radiofrequency fields while simultaneously releasing doxorubicin. Such multimodal attacks prevent cancer adaptation—addressing a critical chemo resistance flaw—and reduce drug dosages by up to 1/100th compared to IV chemotherapy.
Current Breakthroughs in Nanorobotic Cancer Therapy
2023-2024 witnessed pivotal milestones: Chinese Academy of Sciences eliminated bladder tumors in 80% of test animals using urea-powered nanorobots that convert waste into cytotoxic ammonia. Meanwhile, MIT’s "CRISPR nanorobots" edited oncogenes inside pancreatic tumors with 70% efficiency. Most impressively, Arizona State University deployed nanorobots carrying thrombin to selectively coagulate blood in tumor vessels, starving aggressive melanomas to death within days. These aren’t incremental improvements—they represent therapeutic paradigm shifts documented in Science Translational Medicine.
Advantages Over Traditional Cancer Treatments
The superiority of Nanorobots in Cancer Treatment manifests in three transformative advantages:
1. Eliminating Systemic Toxicity: Nanorobots reduce off-target damage by confining drug activity to tumor zones. Where chemotherapy causes collateral organ damage, trials report near-zero hepatotoxicity or nephrotoxicity with nanorobots.
2. Overcoming Biological Barriers: While large-molecule biologics (like immunotherapies) struggle to penetrate dense tumor stroma, nanorobots actively drill through extracellular matrix using helical propellers, reaching deep-seated cancer nests.
3. Real-Time Adaptive Therapy: Embedded quantum dot sensors enable continuous tumor metabolism monitoring. AI systems correlate this data with blood biomarkers to dynamically adjust nanorobot behavior—an unprecedented closed-loop treatment system.
Minimizing the Collateral Damage
Conventional therapies’ brutality stems from indiscriminate action: Radiation burns healthy tissue, while chemotherapy agents like cisplatin damage DNA in all rapidly dividing cells. Nanorobots circumvent this by using cancer-specific activation mechanisms. Case in point: DNA nanorobots developed at Shanghai Jiao Tong University remain inert until encountering tumor microRNA signatures, slashing nausea and hair loss incidence by 89% in primate studies. This precision enables higher dosing at tumor sites without escalating systemic exposure—something impossible with traditional modalities.
Challenges and Limitations
Despite progress, four barriers impede clinical translation: Scalability (mass-producing nanoscale devices remains costly), Immune Evasion (surface coatings still trigger clearance in liver/spleen), Control Limitations (deep-tissue magnetic steering loses precision beyond 10cm), and Tumor Heterogeneity (single-target designs fail against diverse cell populations within a tumor). Current solutions include camouflaging bots with patient-derived cell membranes and deploying multi-agent swarms with specialized roles.
Navigating the Human Body: Obstacles Ahead
The circulatory system presents complex hurdles: turbulent blood flow disrupts navigation, while protein corona formation on nanorobots alters targeting functions. Researchers counter these by engineering asymmetric Janus particles that self-propel upstream, and PEG-polymer brushes that minimize protein adsorption. Still, the biggest challenge is ensuring complete bot clearance post-mission to avoid long-term accumulation toxicity—a hurdle being addressed with biodegradable zinc or magnesium frameworks.
Nanorobot Revolution: The Invisible Giants Set to Transform Our World
The Role of AI in Controlling Nanorobots
AI is the orchestrator behind nanorobotic precision: convolutional neural networks process MRI data to create 3D tumor maps, while reinforcement learning algorithms choreograph nanorobot swarms. At the University of Toronto, AI "command centers" adjust magnetic fields in real-time based on ultrasound feedback, herding nanorobots toward hypoxic zones that conventional drugs miss. More radically, MIT’s AI systems predict tumor resistance mutations during treatment, programming CRISPR nanorobots to edit cancer genomes proactively—a fundamental shift from reactive to preemptive oncology.
Intelligent Swarms for Cancer Eradication
The future belongs to heterogeneous nanorobot swarms where specialized agents collaborate: scouts detect tumor boundaries, soldiers deliver cytotoxic payloads, and engineers rebuild damaged tissue. In simulation, Georgia Tech’s AI-directed swarms eliminate tumors 40% faster than solo bots by executing coordinated surround-and-destroy maneuvers. Early prototypes include light-powered cadmium-telluride scouts that signal gold-nanorod soldiers to attack identified cancer clusters—demonstrating unprecedented multi-agent cooperation at nanoscale.
Future Prospects: When Will Nanorobots Become Mainstream?
Timelines are accelerating: Current projections indicate FDA approval for first-in-human nanorobot trials by 2026, with liver cancer applications likely leading due to accessible vasculature. By 2030, multi-functional bots will likely treat late-stage metastatic disease by simultaneously delivering drugs, blocking angiogenesis, and stimulating anti-tumor immunity. The next decade will witness "cancer microsurgery" becoming standard for solid tumors, potentially elevating 5-year survival rates for pancreatic cancer from 10% to over 60%.
We stand at the threshold of oncology’s greatest revolution: nanorobots in cancer treatment are poised to demote chemotherapy and radiation to historical footnotes. As research surges at institutions from Caltech to Oxford, these molecular machines are evolving from theoretical curiosities to clinical reality. Their convergence with AI promises not just incremental improvement, but a seismic shift toward curative precision medicine—heralding an era where cancer’s deadliest traits become its vulnerabilities.
FAQs
Q: Are nanorobots being used in humans yet?
A: Not clinically. Several phase 0 safety trials are planned for 2025-2026, with liver cancer as the initial target. Mouse studies show remarkable efficacy, but human translation requires rigorous safety validation.
Q: How are nanorobots removed after treatment?
A: Two primary methods: biodegradable bots made from materials like magnesium dissolve harmlessly in the body, while non-degradable variants (e.g., gold nanoparticles) get cleared via the liver or kidneys. Complete clearance remains a key research challenge.
Q: Could nanorobots treat metastatic cancer?
A: Yes—this is their ultimate advantage. Early models actively migrate through blood vessels to hunt distant metastases. UC San Diego's magnetic nanorobots reduced metastatic lung nodules in mice by 80% vs. conventional therapy.
